
April 26, 2024
Menu
Menu
Linking Northern and Central NJ, Bronx, Manhattan, Westchester and CT
Menu


Ask any graduate of Yavneh Academy in Paramus from the past 23 years to recall some of the highlights of his/her elementary education and without

Torah Academy of Bergen County’s Studio 1600 launched its debut album, “Perek Aleph,” in September 2022. Named neatly for the address of TABC, Studio 1600

(Courtesy of YU) “On Oct. 7, Jewish history called. It has asked us to stand up and stand out as Jews. It has asked us

On Sunday April 7, an estimated 7,000 people attended a rally coordinated by the New York Hostages and Missing Families Forum and over 150 partnering

A message sent out by Rutgers University President Dr. Jonathan Holloway to the campus community rejecting BDS and reiterating plans by the university to move

We’ve all heard the cliché that “history is written by the victors.” Well, the world of investing is no different. When it comes to the

If you think NCAA basketball had a great month in March—and it did, with one of the most fun tournaments in years, especially if you

“I’m better than you!” “No, I’m better than you!” “I know more than you do! “No, I know more than you do!” Sounds like children

Noam Nissel, a rising senior at Northeastern University from West Orange is a natural born innovator, so when he noticed his neighbor attaching a makeshift

A few months ago, Steve Fox of Fox Marketing Services received a call late one Friday afternoon. An organization was preparing to send a group

The average job search in the United States, according to Bureau of Labor Statistics data from January, lasts 20.9 weeks. Does that surprise you? If

Elad Movshovitz, founder of Drimia Winery with his wife, Nava, has had a very difficult past year as a winemaker in Susya, a historic area

(Courtesy of STAR-K) As the world leader in certifying Sabbath mode appliances for over 30 years, STAR-K Kosher Certification recently presented several educational seminars at

Spoiler alert: Cottonseed oil appears to be safe, as far as pesticide levels are concerned, from the results of a single test I did. But

As we keep learning more and more about the difficult year had by Israeli winemakers; beginning on October 7 and continuing through as we prepare

Lutali is an Italian restaurant, but the name is even more Italian. Ralph Mohadeb owns Lutali and named it after his wife Tali. He added

Gabe, which wines are you having this year for the four cups? I am asked this question every year, countless times. Does it really matter?

(JNS) Eighteen people, most of them Israeli soldiers, were injured on Wednesday, April 17 when a Hezbollah attack targeted a community center in Arab al-Aramshe

(JNS) The Israeli Cabinet on Wednesday, April 17 unanimously approved a five-year strategic plan to rebuild, develop and strengthen the western Negev communities devastated during

(JNS) The U.N. Security Council’s committee on new members reported on Tuesday, April 16 that it could not reach a consensus on the revived application

(JNS) The negotiations to forge a deal wherein Hamas would free hostages held in Gaza in return for a ceasefire and the release of terrorists

“I thank our friends for supporting Israel’s defense—support both in words and in deeds,” said the PM. “I thank our friends for supporting Israel’s defense—support

והגדת לבנך And you will tell your children: Once we were slaves in a strange land. We were beaten and starved, forced to work until

We live in a digital world where people rely on technology for many aspects of everyday life. For some that includes Torah study. TorahApp, a

It’s no secret that companies from all industries are becoming more reliant on technology these days. We’re moving through an age of rapid digital transformation

Transferring files and emails from Gmail to outlook can be challenging, especially if you are doing it for the first time. For Pete’s sake, I

It is crucial to make a profit in business. There should be precautionary steps that determine how strategically the availability in the market is being

If you’re looking for a job in the airport, check out this list of the 10 best jobs that are available. From customer service to

The M9 Bayonet knife, like all knives in CS:GO, is an extremely rare commodity obtained by unlocking cases. The M9 Bayonet is one of the

Israeli Olympian AJ Edelman and National Champion Jared Firestone are on a mission to triple the size of the Israeli team at the 2026 Winter

Following two shut out wins, RPRY Girls Hockey notched their third consecutive win with a 5-3 victory against Ramaz in their last regular season home

(Noam sports) The Noam Knights completed the YMSSA sweep at the HALB Tournament this past Sunday. The tier two championship was a rematch of the


If you have been following the eighth grade boys RYNJ Jaguars basketball team this season, you would know that you were witnessing something very special.

The Jewish Link and The Humble Toast would like to recognize Avishai Englander as this week’s Sportstar of the Week. The 14-year-old eighth grader at


Ask any graduate of Yavneh Academy in Paramus from the past 23 years to recall some of the highlights of his/her elementary education and without

Torah Academy of Bergen County’s Studio 1600 launched its debut album, “Perek Aleph,” in September 2022. Named neatly for the address of TABC, Studio 1600

(Courtesy of YU) “On Oct. 7, Jewish history called. It has asked us to stand up and stand out as Jews. It has asked us

On Sunday April 7, an estimated 7,000 people attended a rally coordinated by the New York Hostages and Missing Families Forum and over 150 partnering

A message sent out by Rutgers University President Dr. Jonathan Holloway to the campus community rejecting BDS and reiterating plans by the university to move

We’ve all heard the cliché that “history is written by the victors.” Well, the world of investing is no different. When it comes to the

If you think NCAA basketball had a great month in March—and it did, with one of the most fun tournaments in years, especially if you

“I’m better than you!” “No, I’m better than you!” “I know more than you do! “No, I know more than you do!” Sounds like children

Noam Nissel, a rising senior at Northeastern University from West Orange is a natural born innovator, so when he noticed his neighbor attaching a makeshift

A few months ago, Steve Fox of Fox Marketing Services received a call late one Friday afternoon. An organization was preparing to send a group

The average job search in the United States, according to Bureau of Labor Statistics data from January, lasts 20.9 weeks. Does that surprise you? If
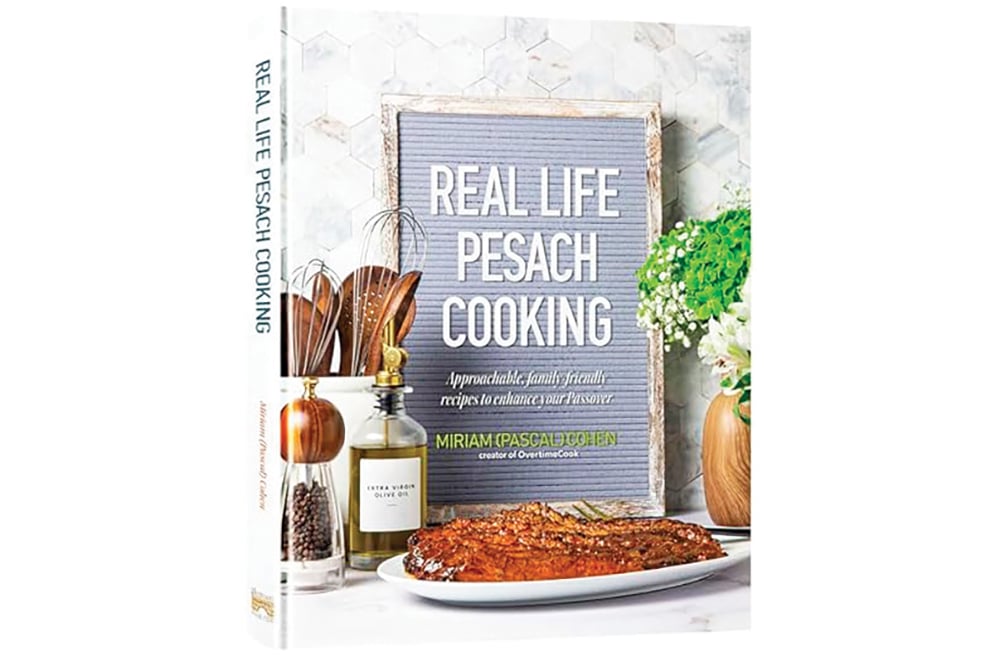
Reviewing: “Real Life Pesach Cooking” by Miriam Pascal Cohen. Mesorah Publications Ltd. 2024. English. Hardcover. 280 pages. ISBN-13: 978-1422639689. We’re close enough to Pesach that

A number of years ago, I went to my good friend Esty Furst for Shabbos Chol Hamoed lunch. In a possibly record-breaking incident, her Pesach

The weeks before Pesach are often fraught with anxiety and pressure to get everything finished on time. There are never-ending to-do lists. And we are

(Courtesy of Manischewitz) Manischewitz, the leading kosher brand for over 130 years, announces a major “rebrand” with a bold fresh look and feel across the

In Jerusalem, as soon as Purim is over, everyone begins to get ready for Pesach. Two and a half weeks ahead, macaroons are already in

The idea of the restaurant was to give patrons a complete white-glove treatment from the moment they walk through the door. There’s even a kind

Chaim Peri (Chaim ben Nechama), 80, has been held captive in Gaza since he was abducted by Hamas terrorists on Oct. 7. He was taken
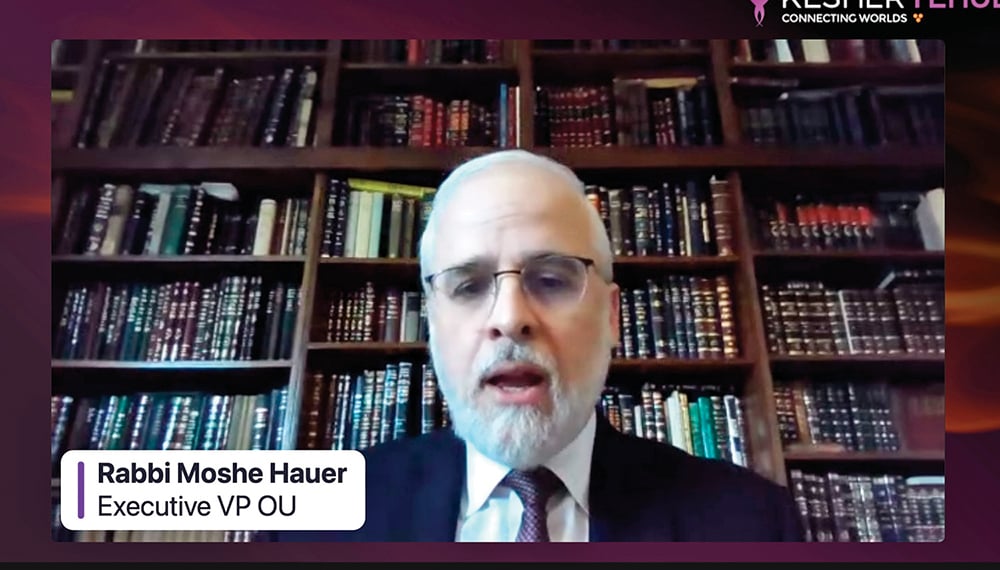
As we prepare for our sedarim this year we are mindful, much more than in years past, that not all Jews are able to celebrate

Matan’s summer program is a unique opportunity to spend three glorious weeks learning and touring with some of the most preeminent and illustrious female Torah

Since its humble beginning in 1975, Laniado Hospital of Netanya, Israel has developed into a modern and extensive medical center in Israel serving a region

Teaneck native Michal Benscher said the program ‘sounds like an amazing option’ that will help many women lead to a more successful transition between seminary

(JNS) An Israeli Air Force strike in the Al-Shati Camp on the northern Gaza coast killed six relatives of Hamas leader Ismail Haniyeh, Arab media

We live in a digital world where people rely on technology for many aspects of everyday life. For some that includes Torah study. TorahApp, a

It’s no secret that companies from all industries are becoming more reliant on technology these days. We’re moving through an age of rapid digital transformation

Transferring files and emails from Gmail to outlook can be challenging, especially if you are doing it for the first time. For Pete’s sake, I

It is crucial to make a profit in business. There should be precautionary steps that determine how strategically the availability in the market is being

If you’re looking for a job in the airport, check out this list of the 10 best jobs that are available. From customer service to

The M9 Bayonet knife, like all knives in CS:GO, is an extremely rare commodity obtained by unlocking cases. The M9 Bayonet is one of the

Israeli Olympian AJ Edelman and National Champion Jared Firestone are on a mission to triple the size of the Israeli team at the 2026 Winter

Following two shut out wins, RPRY Girls Hockey notched their third consecutive win with a 5-3 victory against Ramaz in their last regular season home

(Noam sports) The Noam Knights completed the YMSSA sweep at the HALB Tournament this past Sunday. The tier two championship was a rematch of the


If you have been following the eighth grade boys RYNJ Jaguars basketball team this season, you would know that you were witnessing something very special.

The Jewish Link and The Humble Toast would like to recognize Avishai Englander as this week’s Sportstar of the Week. The 14-year-old eighth grader at